 We’ve now all had the weekend to digest the surprising merger of Express Scripts (NASDAQ:ESRX) and Medco Health Solutions (NYSE:MHS).
We’ve now all had the weekend to digest the surprising merger of Express Scripts (NASDAQ:ESRX) and Medco Health Solutions (NYSE:MHS).I'm going to examine the deal over the next three days. Today, I focus on the marketplace impact and strategic motivations behind the deal. Tomorrow, I'll look at the antitrust challenges, which appear to be different than many people believe. On Wednesday, I'll discuss derivative effects on mid-market PBMs, pharmaceutical wholesalers, and Walgreen (NYSE:WAG).
As I argue below, the deal makes sense given the dynamics of the PBM industry. At the same time, a successful transaction would signal the end of the PBM industry's major growth opportunities and the transition to a more mature, highly consolidated market. The post-2015 world looks much less rosy for PBMs as the generic wave crests and the government crowds out private payers.
Although this is a longer-than-average post, I can only scratch the surface of the many issues surrounding this deal. Pembroke Consulting clients and Gerson Lehrman Group clients can schedule phone calls with me for additional comments beyond what I discuss below.
THE DEAL
Here are key public resources released by the companies:
- Factsheet
- Investor Presentation (July 21, 2011)
- Transcript of 7/21/11 Investor Call
- Agreement and Plan of Merger (Note the following code names: Aristotle=Express Scripts; Plato=Medco.)
 Note that these figures incorporate certain items that won't affect the market until 2012/3:
Note that these figures incorporate certain items that won't affect the market until 2012/3:- Medco’s loss (and Caremark’s gain) of the FEP contract (Interpreting Caremark’s Big Win over Medco)
- Medco’s loss (and OptumRx’s gain) of UnitedHealth (NYSE:UNH) commercial business (source)
- The CVS-Aetna outsourcing deal (CVS-Aetna: Less Than Meets The Eye?)
- CVS’ acquisition of Universal American (CVS-UAM: Part D Powerhouse with a Surprising Alliance)
- Catalyst’s acquisition of Walgreen’s PBM (SOLD! Thoughts on the Catalyst-Walgreen Deal)
Here are my observations on the marketplace factors behind the deal.
The big buyers get bigger. The combination will create a company with greater negotiating leverage against other participants in the pharmaceutical system. (See pages 24-30 and 43-45 of The 2010-11 Economic Report on Retail and Specialty Pharmacies for background.)
- Generic manufacturers, which sell drugs to PBM mail pharmacies
- Brand-name manufacturers, which negotiate rebate and discount contracts
- Pharmacies, which negotiate network agreements
- Wholesalers, which supply brand-name drugs to PBM mail pharmacies
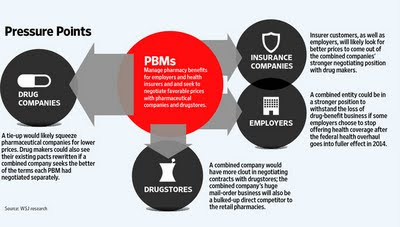 Folks, it's called an oligopsony, not a monopoly. More on this topic tomorrow.
Folks, it's called an oligopsony, not a monopoly. More on this topic tomorrow.Synergies in the Generic Wave. The PBMs want scale going into the big wave of newly-generic drugs, especially since the launch period provides maximum generic profitability for everyone in the drug channel (PBMs, pharmacies, and wholesalers). See Medco’s generic forecast from last November in Medco's Generics Outlook: Party On, Dudes!
The companies project $1 billion in synergies when fully integrated, but that seems low to me. CVS Caremark claimed more than $700 million in total cost synergies in 2008 from their combination. (source) The majority of those savings came from generic drug purchasing—both sheer volume as well as contract comparisons. Prasco is a cautionary tale for generic manufacturers from the CVS Caremark merger. See CVS' Channel Power.
The Post-2015 Problem. The generic wave peters out by 2015, so the PBMs have a business model problem. Plus, the superior profits from generic drugs are catching the attention of payers and retail competitors. When the generic dispensing rate hits 85% in 4-5 years, payers—both government and commercial—will look even harder at channel profits on generics as a way to reduce drug spending. This countervailing force pushes against per-script profit growth, suggesting a lower-cost platform is a key to success in the post-2015 future.
The old world of brand-name formulary access and rebate negotiations is rapidly fading as generics come to dominate traditional drugs. In a world of low-cost generics, the quality of care—adherence, compliance, appropriate utilization—becomes much more important than the unit price per pill. Hence, PBMs need to offer programs to payers that emphasize clinical and health care services intended to improve patient outcomes and lower the client’s total health care costs. A larger company can invest more (and risk more) in developing these new services.
Meet the new boss. Health care reform provides the prospect of expanding pharmacy benefit insurance to the uninsured. In theory, PBMs will ride this wave to more growth. (See Health Reform: Impact on Drug Channels and Health Care Reform and Pharmacy Benefit Premiums.) However, this growth comes with the downside of substantial government involvement, especially if the commercial market shrinks in favor of insurance exchanges. (See Will Exchanges Crowd Out Employer Coverage?) We've already seen both state and federal governments require increasing degrees of transparency, so the new world may not be as good for PBMs as the old world.
This is an acquisition, not a merger. The new board of directors will include Express Scripts’ entire board plus two people from Medco’s board. Medco pursued ideas that never appealed to Express Scripts. These initiatives will likely be minimized or spun-out of the new company. Examples include:
- United BioSource (Is Medco Overreaching with United BioSource?)
- European expansion (Medco Expands in Europe)
- Pharmacogenomics (Medco's Pharmacogenomic Future)
Tune in tomorrow for more. Same bat time! Same bat channel!

